Situations When Parents Should Consider IVF Options

Anyone can suffer from infertility issues. If you are also facing this condition then becoming a parent can be difficult for you. Many couples face infertility issues for one or both partners. Dreaming of being a parent to a child is not possible without medical help. This is where IVF comes into play. This is […]
The Harmony Test

During pregnancy our surrogate mothers will make a lot of tests and screenings that can be tiring and irritating. That is why we want you to know about the importance and necessity of one of the most important tests that you can make during this precious period. We think that for every parent and also […]
My surrogate mother will give birth soon: what should I care about?

So, there are only a few more steps to become parents. First of all, our congratulations! This point is probably the most worrying part of the whole pregnancy period, so we decided to write a small reminder to you to relief the possible stress. Planning your second visit Few weeks to a few months before […]
Male infertility
The reproductive system is a complex mechanism, any detail of which may be impaired due to various pathologies. According to the U.S. National Institutes of Health, near 50% of male infertility causes cannot be determined. Here we will describe a few of the known causes to increase your awareness and your chances to overcome it. […]
Causes of female infertility

Nowadays problems with having babies increase enormously. Sometimes causes of female infertility are not so evident, and woman starts to ask herself “Why I cannot become pregnant?”. Today we will talk about some reasons of female infertility and timely response to it. What is an infertility? According to World Health Organization, infertility is an inability […]
Egg Puncturing

In vitro fertilization (IVF) is a complex series of procedures used to treat infertility or genetic problems and assist with the conception of a child. It is the most effective form of assisted reproductive technology. The procedure can be done using your own eggs and your partner’s sperm. Or IVF may involve eggs, sperm or […]
Euploidy and aneuploidy
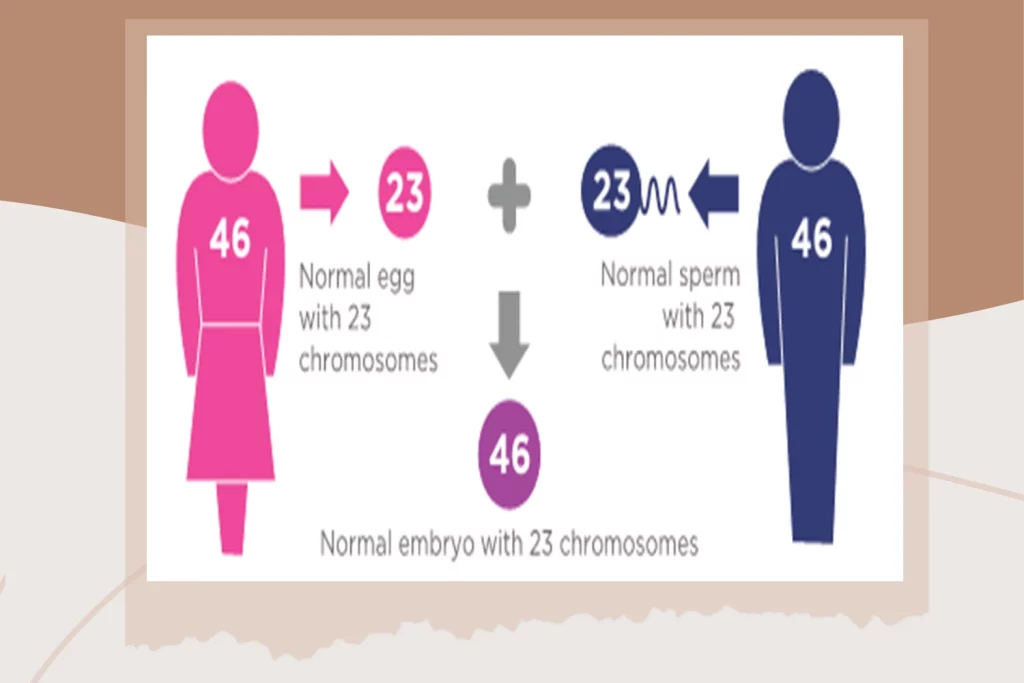
Euploidy and aneuploidy It is very important to receive good quality embryos during the artificial reproductive technologies, as it is the key to a successful treatment. But what does actually “good quality” mean? Is this about the microscopical evaluation of embryos by an embryologist? Let’s go to the fundamentals of this question. During […]
Folic acid for pregnant women

Folic acid for pregnant women Folic acid helps prevent defects of neural tube, which affect the brain (anencephaly) and spinal cord (spina bifida), also it affect the baby’s heart. Neutral tube defects can develop at the first 28 days after conception. Most of the time, the woman doesn’t even know that she is pregnant. More […]
How to prevent and protect women from Infectious diseases Toxoplasmosis during Pregnancy

How to prevent and protect women from Infectious diseases like Rubella and Toxoplasmosis during Pregnancy to avoid complications Today, in most of countries, the majority of infectious diseases are eradicated as a result of vaccination and decades of efforts of the medical professionals. Such fatal infections like tetanus, rabbis and smallpox are very rare and people can […]
What are the risks of preeclampsia & eclampsia for pregnant women?

What are the risks of preeclampsia & eclampsia for pregnant women? Preeclampsia and eclampsia continue to be major contributors to maternal mortality and morbidity. Lack of appreciation for the multi‐organ involvement of preeclampsia, combined with overly rigid criteria for diagnosis, may hinder early diagnosis. Pons Medical Group Pons Medical Group is a leading surrogacy agency […]
