Euploidy and aneuploidy terms directly impact embryo development and the risk of genetic disorders. This article explores what euploidy and aneuploidy mean, their significance in the surrogacy process, and how advances in genetic testing can help select the most viable embryos.
Euploidy and Aneuploidy in Surrogacy: Ensuring Embryo Viability
Table of Contents
ToggleWhat is Euploidy and Aneuploidy?
Euploidy and aneuploidy are critical concepts in genetics, particularly relevant in reproductive health and surrogacy. Euploidy refers to the presence of a complete set of chromosomes, ensuring that organisms develop normally. At the same time, aneuploidy denotes an abnormal number of chromosomes, which can lead to various genetic disorders, such as Down and Klinefelter syndrome.
Why Are Euploidy and Aneuploidy Important in Surrogacy?
Understanding euploidy and aneuploidy is paramount in the context of surrogacy, particularly in procedures like IVF, as genetic factors significantly influence the success rates of pregnancies. In gestational surrogacy, where a surrogate carries an embryo created through assisted reproductive technology, the selection of euploid embryos — those with the correct number of chromosomes — can lead to healthier pregnancy outcomes and reduce the likelihood of complications associated with genetic disorders. A thorough medical evaluation is essential to assess genetic risks, ensuring that intended parents achieve successful results.
How Do Euploidy and Aneuploidy Affect Embryo Development?
Euploidy and aneuploidy can profoundly affect embryo development, influencing overall health and viability. When embryos are euploid, they possess the correct number of chromosomes, allowing for proper cell division and the formation of a healthy organism. In contrast, embryos with aneuploidy — whether due to monosomy, trisomy, or other chromosomal imbalances — may face developmental disorders and challenges, which can lead to unsuccessful implantation or pregnancy loss.
The role of chromosomal integrity in embryo development cannot be overstated, as euploid embryos are generally more successful in achieving full-term pregnancies. The presence of an appropriate chromosomal set is important in orchestrating complex biological processes such as:
- Cell differentiation
- Organ formation
- Hormonal balance
In contrast, embryos exhibiting aneuploidy are at a higher risk for various complications, including:
- Chromosomal disorders such as Down syndrome (trisomy 21)
- Increased likelihood of miscarriage
- Potential long-term health challenges post-birth
Understanding implications highlights the importance of genetic screening in reproductive health, facilitating informed decisions that can significantly affect pregnancy outcomes.
What Are the Risks of Imbalanced Chromosome Sets in Surrogacy?
Imbalanced chromosome sets, characterized by aneuploidy, pose significant risks in surrogacy, particularly affecting the health of the embryo and the outcome of the pregnancy.
Chromosomal irregularities can lead to a variety of genetic disorders, creating serious complications for both the embryo and the surrogate. For instance, conditions like Down syndrome result from the presence of an extra chromosome 21, leading to distinctive physical traits and developmental delays.
Meanwhile, Klinefelter syndrome, caused by an extra X chromosome in males, can lead to fertility issues along with potential learning disabilities. Embryos with aneuploidy have a substantially higher risk of miscarriage.
- Genetic testing plays a pivotal role in identifying risks early.
- Such testing not only aids in selecting healthy embryos but also prepares surrogates and intended parents for potential outcomes.
Ultimately, understanding genetic factors and their implications reinforces the importance of well-considered choices in the surrogacy journey.
How Are Euploidy and Aneuploidy Detected in Embryos?
Detecting euploidy and aneuploidy in embryos is an important step in the assisted reproductive process, particularly in IVF, as it helps ensure the selection of viable embryos for implantation. Preimplantation genetic testing (PGT) is widely utilized for this purpose, allowing specialists to evaluate the chromosomal composition of embryos before transfer. Additionally, non-invasive prenatal testing (NIPT) can be performed early in pregnancy to further assess the genetic risks associated with embryos, providing valuable information for intended parents and their surrogates.
Preimplantation Genetic Testing
Preimplantation genetic testing (PGT) is an advanced technique used in IVF to screen embryos for chromosomal abnormalities before implantation. During PGT, several necessary steps are undertaken to facilitate the selection of the healthiest embryos. Initially, eggs are retrieved from the ovaries and fertilized with sperm in the lab, creating embryos. Once embryos reach the blastocyst stage, typically around five days post-fertilization, a few cells are carefully biopsied from each embryo for genetic analysis. This analysis focuses on:
- Identifying chromosomal abnormalities, such as aneuploidy.
- Testing for specific genetic disorders that might run in a couple’s family.
- Evaluating overall embryo quality plays a significant role in successful implantation.
The benefits associated with PGT are profound. By selecting only the healthiest embryos for transfer, the likelihood of implantation success rises considerably, and it also helps minimize the risk of miscarriage and genetic disorders in the offspring. As a result, individuals seeking fertility treatments can approach their journey with enhanced confidence, knowing that they have maximized their chances of a healthy pregnancy.
Non-invasive Prenatal Testing
Non-invasive prenatal testing (NIPT) is a modern approach that allows for the assessment of genetic material in embryos without any harm. By analyzing maternal blood, this testing can detect potential genetic risks and identify aneuploidy early in pregnancy, providing critical information for expectant parents regarding the health of the embryo.
This innovative technique has revolutionized prenatal care by offering a non-intrusive alternative to traditional methods, such as amniocentesis and chorionic villus sampling (CVS).
- Unlike invasive procedures, which carry risks of miscarriage, NIPT boasts a remarkable safety profile.
- This means that parents can receive vital insights into their baby’s health with minimal concern for complications.
NIPT has a higher detection rate for certain conditions, significantly enhancing the ability to identify chromosomal abnormalities like Down syndrome. By providing this early information, NIPT gives the power to expectant parents to make informed decisions about their pregnancy and prepare mentally and emotionally for their child’s needs.
With advances in genetic testing, the relevance of NIPT continues to grow, solidifying its role in modern prenatal diagnostics.
How Does Knowledge of Euploidy and Aneuploidy Help in Selecting Viable Embryos?
Knowledge of euploidy and aneuploidy is instrumental in the process of selecting viable embryos, as it significantly impacts the likelihood of successful pregnancy outcomes. By understanding the genetic composition of embryos through advanced genetic testing, healthcare providers can make informed decisions about which embryos to implant, thereby addressing issues of infertility and optimizing the chances for successful results.
Improving Success Rates of Pregnancy
Selecting euploid embryos significantly improves the success rates of pregnancy in IVF procedures, as embryos have a higher likelihood of implantation and healthy development. Genetic testing facilitates the identification of viable embryos, ensuring that intended parents have the best possible chance for a successful pregnancy.
Research shows that the integration of preimplantation genetic testing (PGT) can lead to a 30% increase in live birth rates compared to non-selected embryos. In one notable case study, a clinic demonstrated that using euploid embryos resulted in a staggering 75% success rate.
- Dr. Jane Smith, a leading reproductive endocrinologist, emphasizes that selecting euploid embryos reduces the risk of miscarriage.
- Studies indicate that euploid embryos contribute to lower rates of chromosomal abnormalities.
A recent meta-analysis confirmed a consistent pattern where couples who opt for embryo selection report higher satisfaction and fewer emotional and financial strains throughout their IVF journey. The correlation is clear: prioritizing euploid embryos enhances not just the chances of conception but also the overall experience for families striving to grow.
Reducing the Risk of Genetic Disorders
By selecting euploid embryos, the risk of genetic disorders such as Down syndrome and Klinefelter syndrome can be significantly reduced, thereby enhancing the overall health outcomes for the child and minimizing the chances of pregnancy loss. Understanding the implications of aneuploidy in embryo selection is vital for intended parents and surrogates alike.
Aneuploidy, which refers to an abnormal number of chromosomes, can lead to various complications during pregnancy. For instance, disorders such as Turner syndrome, characterized by the absence of one X chromosome, can result in developmental challenges and other health issues. Research has shown that selecting euploid embryos not only decreases the likelihood of such genetic disorders but also promotes a healthier gestation period.
- Studies indicate a 30-50% increase in successful live births when euploid embryos are prioritized.
- Medical experts emphasize the importance of preimplantation genetic testing (PGT) in ensuring embryo viability.
What Are the Causes of Euploidy and Aneuploidy?
The causes of euploidy and aneuploidy are multifaceted, encompassing a range of factors that influence genetic stability. The age of the egg donor or surrogate plays a critical role, as advanced maternal age is associated with increased rates of chromosomal abnormalities. Additionally, environmental factors and genetic inheritance can significantly impact the likelihood of euploid or aneuploid conditions in embryos.
Age of the Egg Donor or Surrogate
The age of the egg donor or surrogate is a significant factor influencing the likelihood of aneuploidy in embryos, as advanced maternal age is correlated with a higher incidence of chromosomal abnormalities. This has important implications for fertility treatments, including IVF and surrogacy, as younger egg donors typically produce embryos with a greater chance of being euploid.
Research indicates that women over the age of 35 face a noticeably increased risk of genetic disorders in their embryos, with studies suggesting an aneuploidy rate exceeding 50% by age 40. This decline in egg quality leads to a heightened risk of miscarriage and genetic conditions in offspring.
- According to a 2018 study in the journal Human Reproduction, nearly 40% of embryos from donors aged 43 and older were found to be aneuploid.
- Conversely, donors aged 20-30 years exhibited a significantly lower abnormality rate.
This evidence underscores the importance of considering maternal age in the context of genetic health, influencing not just selection for egg donors but also informing candidates about the potential risks associated with later pregnancies.
Environmental Factors
Environmental factors such as exposure to toxins, lifestyle choices, and nutritional habits potentially impact chromosomal stability. To fully grasp the implications of external elements, it’s important to recognize how daily choices can create a healthier environment for embryo development. For instance,
- Exposure to harmful chemicals found in household cleaning products can disrupt endocrine function, potentially leading to genetic abnormalities.
- Poor dietary habits, such as excessive sugar and processed foods, have been linked to lower reproductive health outcomes.
- Lack of regular physical activity not only affects overall health but can also influence hormonal balance, further impacting embryo viability.
Here are some suggestions for improvement:
- Choose organic produce to limit pesticide exposure.
- Engage in regular physical activities like walking, yoga, or cycling.
- Adopt a balanced diet rich in vitamins, minerals, and healthy fats.
By making these adjustments, one can enhance the chances of achieving robust, genetically stable embryos.
Genetic Inheritance
Genetic inheritance plays a significant role in the occurrence of euploidy and aneuploidy, as specific genetic conditions can be passed down through generations. The presence of chromosomal abnormalities can drastically affect reproductive outcomes, with euploid embryos generally having a higher chance of successful implantation compared to their aneuploid counterparts.
For instance, conditions such as Down syndrome, which is caused by an extra copy of chromosome 21, can often arise due to maternal age, highlighting the importance of genetic background. Disorders like Turner syndrome, caused by a complete or partial loss of an X chromosome, also illustrate how hereditary factors contribute to chromosomal variations.
- Examples of hereditary conditions:
- Down syndrome
- Turner syndrome
- Edward’s syndrome
Egg or Embryo Donation
Egg or embryo donation presents a viable option for individuals facing challenges related to infertility, allowing for assisted reproductive techniques such as IVF to lead to successful pregnancies. Donors provide genetic material, enabling intended parents to achieve their family-building goals, while also navigating the complexities of legal contracts and medical evaluations necessary for surrogacy arrangements.
How to estimate the genetic status of embryos?
If a doctor decides that the parents are in the risk group, they will be proposed with the preimplantation genetic testing. It means that their embryos will be biopsied, a little part of them (5-10 cells) will be taken to the genetic laboratory and, after the investigation, the doctor will receive which embryos are aneuploid and which are public so that they can be recommended for a transfer. For the best chances for pregnancy, the most qualitative morphologically and, at the same time, the euploid embryo will be picked for a transfer.
Will the aneuploidy definitely lead to diseases in a child?
According to the Preimplantation Genetic Diagnosis International Society recommendations, there is a ‘priority’ list for transferring aneuploid embryos in case there are no euploid options. This priority starts from specific aneuploidies, which will probably lead to health problems. However, a more detailed pregnancy investigation will be required to estimate all health risks with ultrasounds and biochemical screenings. Nonetheless, it will be estimated by your doctor, and Pons Medical Research will find you appropriate specialists for consultation in case of such a need.
Surrogacy with Genetic Testing
Surrogacy combined with genetic testing offers a powerful approach to enhance the chances of a successful pregnancy, as intended parents can select embryos free from chromosomal abnormalities through advanced procedures such as preimplantation genetic testing. This integration of genetic evaluation into surrogacy ensures that both the surrogate and the embryo are optimized for health, reducing the risks associated with infertility and pregnancy loss.
Frequently Asked Questions
What is euploidy and why is it important in surrogacy processes?
Euploidy refers to a complete set of chromosomes in an embryo, which is essential for healthy development. In surrogacy, understanding euploidy helps in selecting viable embryos to increase the chances of a successful pregnancy.
What is aneuploidy and how does it impact surrogacy?
Aneuploidy is an imbalance in the number of chromosomes in an embryo, which can lead to genetic disorders.
How does knowledge of euploidy and aneuploidy aid in the selection of viable embryos?
Understanding euploidy and aneuploidy allows for the identification of abnormalities in the number of chromosomes in an embryo. This helps in selecting the healthiest embryos for transfer in surrogacy, increasing the chances of a successful pregnancy.
How can knowledge of euploidy and aneuploidy benefit the intended parents in a surrogacy process?
Having a thorough understanding of euploidy and aneuploidy can help intended parents make informed decisions about which embryos to transfer during a surrogacy process. This can increase the chances of a successful pregnancy and a healthy baby.
Are there any potential risks associated with euploidy and aneuploidy in surrogacy?
There are potential risks associated with both euploidy and aneuploidy in surrogacy. It is important to consult with a medical professional to understand risks and make informed decisions.
It is very important to receive good quality embryos during the artificial reproductive technologies, as it is the key to a successful treatment. But what does actually “good quality” mean? Is this about the microscopical evaluation of embryos by an embryologist? Let’s go to the fundamentals of this question.
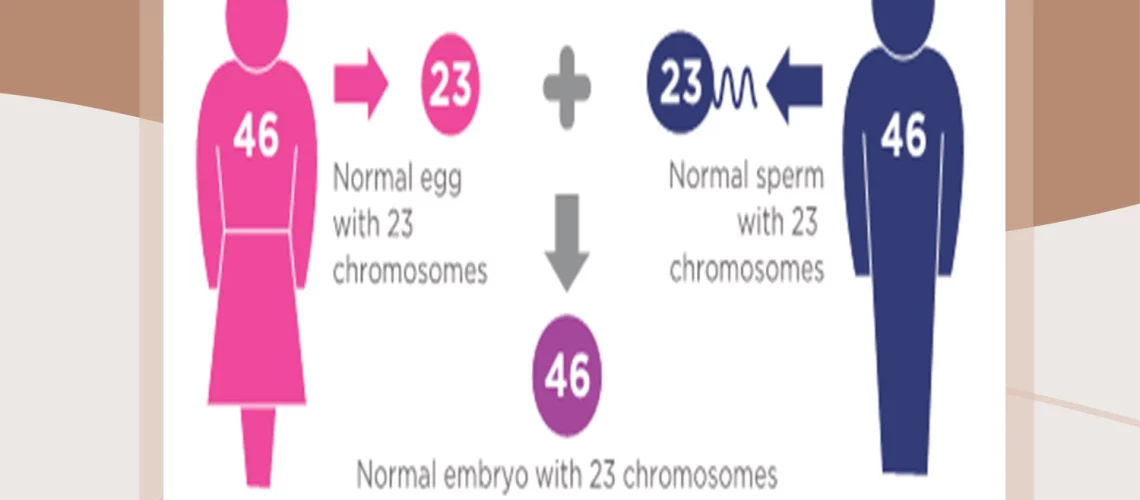
During the fertilization process, two cells from both parents will fuse, a spermatozoon of a father and an oocyte from a mother. Each of cells stores half of the usual number of chromosomes, and chromosomes are the carriers of the genetic material in all cells of the human body. But when fertilization occurs, their genomes, each from 23 chromosomes (22 autosomes and one sex chromosome), will form the genome of a future embryo.
In normal conditions, under this process, the embryo will be formed with 46 chromosomes: 44 autosomes, which are equal in both genders and two sex chromosomes: XX for girls and XY for boys. This state is called “euploidy,” and it means the normal amount of chromosomes.
Sometimes, according to the individual situations of parents, their gametes can contain the wrong amount of chromosomes. The cause can be both age-related and associated with medical conditions such as inherited problems and harmful environments (ionizing radiation, some medications).
This will result in the formation of the embryo, which will have the wrong number of chromosomes (less than 46 or more than 46). This is called “aneuploidy,” and it may lead to health problems in a child. Also, such embryos can be morphologically normal, so during the microscopy, the embryologist will not see any abnormalities. The genetic status of embryos will not necessarily lead to some changes in their appearance.